[PART I – MYSTERIES]
[PART II – CURRENT THEORIES OF OBESITY ARE INADEQUATE]
[PART III – ENVIRONMENTAL CONTAMINANTS]
[INTERLUDE A – CICO KILLER, QU’EST-CE QUE C’EST?]
[PART IV – CRITERIA]
[PART V – LIVESTOCK ANTIBIOTICS]
[INTERLUDE B – THE NUTRIENT SLUDGE DIET]
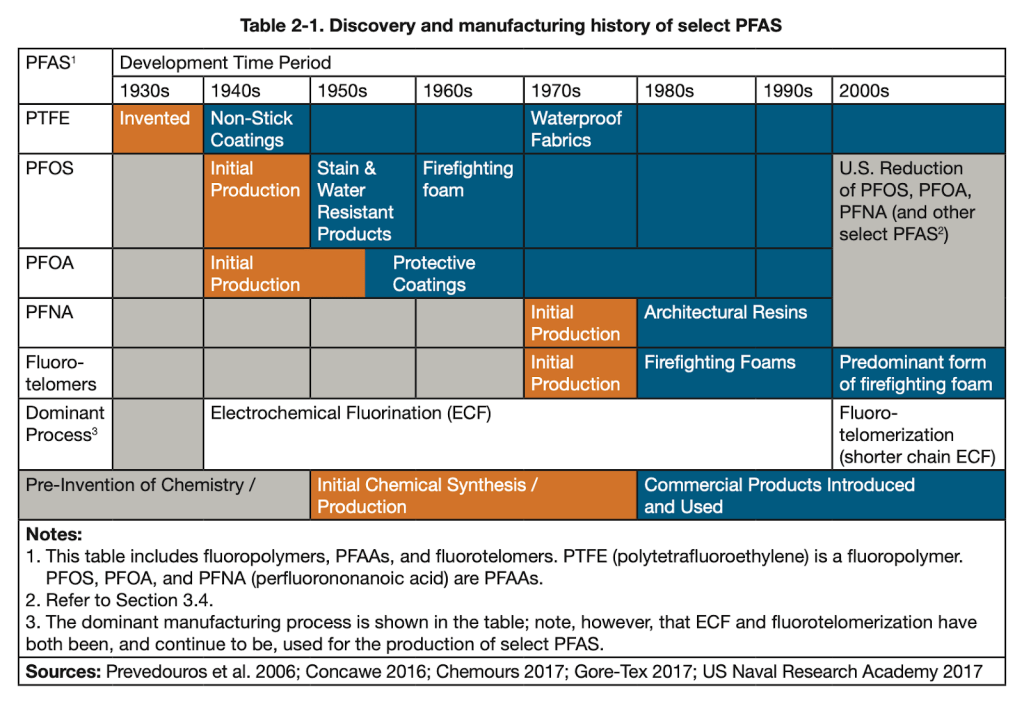
[PART VI – PFAS]
Lithium is the third element on the periodic table, the lightest metal, a hit Nirvana single, and a mood-stabilizing drug often used to treat bipolar disorder.
Lithium isn’t synthetic, of course, but it can still be an environmental contaminant. While it occurs naturally in small concentrations in groundwater, human activity might have led to serious increases over the past few decades.
Unlike the other contaminants we’ve reviewed, we don’t need to spend any time convincing you that lithium makes people gain weight: it does. Almost everyone who takes lithium at therapeutic levels gains some weight. About half of them report serious weight gain, on average 22 lbs (10kg), and about 20% of patients gain more than that. Weight gained is correlated (r = .44, p < .001) with dosage. Unsurprisingly, weight gain on lithium is related to an increase in leptin levels.
We’d love to tell you whether lithium concentrations in groundwater have increased over time. But while lithium is easy to detect, assessing lithium levels is not a part of the standard analysis of drinking water, so we don’t have reliable historical data to work with. There aren’t even EPA standards for lithium levels in drinking water.
We’d also like to tell you about how much lithium people are exposed to, and whether that has increased over the past several decades. Measuring serum lithium is relatively easy, and people who are starting lithium treatment get checked frequently to make sure that their blood levels aren’t too high. Despite this, there doesn’t seem to be any data on serum lithium levels in the general population. The NHANES data has records of how much uranium there was in your urine every year from 2000-2016, but not a single measure related to lithium. Great job, guys.
We can’t talk about trends in the groundwater or in people’s bodies directly. But what we can do is look at other trends that we would expect to be related. For example, this figure shows a graph of USGS-reported records for global lithium production since 1900:
This graph is pretty telling. Almost no lithium was produced before 1950, so human activity couldn’t have been adding a meaningful amount to the groundwater back then. Serious lithium production started around 1950, which could help explain why obesity went from about 3% in 1890 to about 10% in 1980, but we see that lithium production truly spikes around 1980. While there have been a few ups and downs, production has as a rule continued to rise ever since. This graph only goes up to 2007, but USGS and other sources confirm that production has continued to increase, at about 11% per year from 2007 to 2017.
Lithium definitely ends up in the groundwater. It’s there in small concentrations naturally, but human activity adds more. In Seoul, South Korea, lithium concentrations sextuple as the Han river passes through the city’s densest districts. This is reflected not only in the river, but also in the tap water in the city — tap water from sites further along the river’s course have similarly elevated lithium levels.
This suggests that rivers pick up lithium along their course and generally have higher lithium levels as they flow downhill. This is supported by data from Austria, which shows that lithium levels in drinking water vary systematically with altitude, with higher concentrations of lithium found in districts at lower altitudes:
We should note that a paper looking at groundwater in the United States from 1992-2003 found the opposite effect: higher levels of lithium at higher altitudes. “However,” they say, “these findings should be interpreted with caution.” We agree. There are 3,141 counties in the United States, and they only looked at data from 518. They only examined data from 15 states, most of them states at relatively low elevation. These weren’t randomly selected, either; they were the sites with the highest number of lithium samples in the years 1992-2003.
We’ve already discussed the issues that come up when you conduct analysis on a restricted range of data. Further, the Seoul data shows that lithium levels spike around urban areas. If some of the high-altitude measurements were near or immediately downstream from cities or manufacturing areas, that might make it look like higher-altitude locations have higher levels of lithium on average.
Dosage
The therapeutic dose of lithium in blood serum is usually considered to be in the range of 0.8 – 1.2 mmol/L, though some sources suggest that lower doses are more effective, with the “minimum efficacious serum lithium level” being possibly as low as 0.4 mmol/L. To translate these to more familiar terms, 0.8 mmol/L is about 5600 ng/mL, and 0.4 mmol/L is about 2800 ng/mL.
That’s quite a lot. In comparison, lithium levels in groundwater rarely exceed 200 ng/mL. But perhaps surprisingly, even very low levels can have an influence on our health and mental states. One study examining data from 27 Texas counties between 1978-1987 found that rates of suicide and homicide (as well as other forms of violent and impulsive behavior) were negatively correlated with lithium in drinking water, over water lithium levels ranging from 70 to 170 ng/mL. Another study looking at various cities in Lithiuania (no relation to lithium) found a negative relationship between lithium exposure and suicide. The lithium levels in the public drinking water systems they examined ranged from 0.5 to 35.5 ng/mL, with a median level of 3.6 ng/mL. In general, reviews of this literature find that trace levels of lithium have a meaningful impact on behavior.
There’s only one randomized controlled trial examining the effects of trace amounts of lithium, but it finds the same thing. A group of former drug users (heroin, crystal meth, PCP, and cocaine), most of them with a history of violent crime or domestic violence, were given either 400 µg per day of lithium orally, or a placebo. For comparison, a normal clinical dose is 300,000 – 600,000 µg, taken two to three times per day. Even on this comparatively tiny dose, everyone in the lithium group reported feeling happier, more friendly, more kind, less grouchy, etc. over a four week period, “without exception”.
(These former drug users didn’t have normal moods to begin with — one said “I am always extremely moody and fight with my girlfriend frequently” before he was treated — so it’s not clear if trace amounts of lithium would improve mood in everyone else. Similarly, therapeutic doses are only given to patients with bipolar disorder, and it’s not clear what the effects would be on someone without this diagnosis.)
In the placebo group, people were just about as grouchy as before. When they switched the placebo group over to lithium, these people responded in exactly the same way.
This is pretty strong evidence that even very small doses of lithium can have meaningful effects. So should we be surprised that they don’t mention any weight gain? There isn’t much data on the time course of weight gain in lithium treatment, but it seems to come on pretty fast. In one study with normal therapeutic doses, 15 bipolar inpatients gained an average of 13 lbs (5.9 kg) over six weeks. While the sample size is quite small, this tells us that sometimes a lot of weight gain can happen fast.
We don’t think this is a huge problem. The randomized controlled trial on trace exposure only lasted a couple of weeks. Even if patients were gaining weight at the same rate as patients on a therapeutic dose, they might not have noticed. The researchers didn’t intend to examine weight gain, and probably didn’t measure it. They don’t report any other side effects. Heroin, crystal meth, PCP, and cocaine all make people lose weight, so it’s possible that weight gain in the former drug users would be seen as a sign of health. It’s also worth noting that while these trace amounts do appear to have real, consequential effects, the dosage was about 1,000 times smaller than a therapeutic dose. In this situation, it’s not crazy to think that weight gain might take a few weeks or even months to manifest. We see a version of the main effect — improved mood — in this tiny dose. It seems reasonable that we might see a version of this side effect as well.
This study can give us a lower limit not only of the dosage, but by extension, of the minimum effective serum level. As a ballpark estimate, therapeutic dosages are in the range of 1,000,000 µg per day and they lead to serum levels of around 5000 ng/mL. This means the 400 µg per day dose from the randomized controlled trial would lead to a serum level of around 2 ng/mL. Other sources suggest that blood levels may end up slightly higher on low doses. For example, doses in the range of 385 to 1540 µg per day lead to serum levels around 7 to 28 ng/mL. One study testing serum lithium as a compliance marker for food and supplement intake found that giving people lithium-tagged yogurt with a dose of about 1000 µg per day over a period of six weeks led to an increase in serum levels from 6 ng/mL to 46 ng/mL.
These papers disagree on the specifics but they agree on the general picture. A serum level in the range of 10 ng/mL is enough to influence mood, and a dose of about 400 µg per day is enough to get you there. Whether lower doses have an effect is unclear, but we should certainly be interested in numbers in these ranges and up.
Trace Exposure
There aren’t any other randomized controlled trials, but if trace amounts are enough to cause obesity, then we should see relationships between trace lithium levels and obesity rates.
In Texas, a survey of mean lithium levels in public wells across 226 counties (Texas has 254 in total) found lithium levels ranging from 2.8 to 219.0 ng/mL. Now Texas is not one of the most obese states — but it tends to be more obese along its border with Lousiana, which is also where the highest levels of lithium were reported.
West Virginia and Alabama, on the other hand, are two of the most obese states in the nation. We haven’t been able to find any reliable groundwater concentration data for these states, but we can certainly note that both of them have problems with lithium contamination coming from local mining operations. And it’s not just Alabama and West Virginia — other states are facing similar contamination.
In Greece, lithium levels in drinking water range from 0.1 ng/mL in Chios island to 121 ng/mL on the island of Samos, with an average of 11.1 ng/mL. Unfortunately there’s not much data on the prevalence of obesity in Greece, but we can conduct some due diligence by checking a few of these endpoints. Samos, with the highest levels, is the obvious place to start. On Samos, 10.7% of children aged 3-12 are overweight, compared to 6.5% on the island of Corfu. A full 27% of high schoolers on Samos island were overweight in 2010, and 12.4% were obese. In comparison, about 12.5% of American high schoolers were obese in the same period.
In the Caspian Sea, lithium concentrations are 280 ng/mL. As we’ve already reviewed, some of the most obese provinces in Iran border the Caspian. The Dead Sea has concentrations even higher, at 14,000 ng/mL, but for the obvious reasons, we don’t think people are getting a lot of their drinking water from the Dead Sea. On the other hand, obesity in the West Bank is pretty high — as high as 50% in men in 2003!
Very high concentrations of lithium have also been reported in Austria. For the most part, Austria has normal amounts of lithium in its drinking water, around 13 ng/mL. But in the east, the concentrations are much higher. In the Mistelbach district, the average level of lithium in the drinking water was 82 ng/mL, and the highest single measurement was near Graz, at 1300 ng/mL. Both of these are in eastern Austria, where obesity levels are highest. Mistelbach in particular is one of the most obese districts in the country.
Chile and Argentina are the most obese countries in South America (28% each) and are two of the biggest exporters of lithium in the world. Unsurprisingly, this is reflected in their groundwater.
In northern Chile, lithium levels in the groundwater can reach levels 10,000 times higher than normal. The rivers running through many small valleys see lithium concentrations of 600 – 1600 ng/mL. The drinking water in many towns has levels up to 700 ng/mL. And in the headwaters of the Rio Camerones, lithium hits concentrations of 24,880 ng/mL. In 1980, Zaldivar reported similar levels of lithium in the groundwater, stating that they were “the highest reported in the world”. He also measured serum levels in people at these different sites, and found values ranging from 22.3 ng/mL to 85.8 ng/mL.
(“We tried to find Zaldivar to learn more about his work,” says a later paper, “but to no avail. He left Chile when Pinochet came to power and effectively disappeared.”)
In Argentina, lithium can reach up to 1000 ng/mL in drinking water, and the locals end up with a lot of exposure. At the site with the highest levels, lithium concentrations reached an average of 4,550 ng/mL in people’s urine. The highest level in someone’s urine was actually a whopping 14,300 ng/mL. The locals seem to be getting much of their lithium exposure from their tap water, as the amount of lithium in urine was correlated with the number of glasses of water consumed per day (r = 0.173, p = 0.029).
These are all freshwater levels. In seawater, lithium concentrations are reliably quite high, ranging from 100 ng/mL to over 1000 ng/mL. Now, most people are not actually drinking meaningful amounts of seawater, but if you live near the ocean, you might still be exposed indirectly.
One mystery we haven’t mentioned yet is that the Middle East is extremely obese (see map below), one of the most obese regions on earth. Jordan, Qatar, Libya, Egypt, Lebanon, and Saudi Arabia all barely trail the United States in terms of obesity, and Kuwait is actually slightly more obese than the United States, about 38% obese compared to 36% in America. These countries are very dry, and so all of them get a lot of drinking water from desalinated seawater. Saudi Arabia gets about half of its drinking water from desalination and is one of the most obese nations on earth. Kuwait built its first desalination plant in 1951, and has actually been one of the most obese countries in the world for a long time. Back in 1975, when the rate of obesity in the United States was around 10%, the rate of obesity in Kuwait was about 18%.
Desalination removes all trace elements from seawater, but because distilled water corrodes metal pipes and trace elements are important to health, the desalinated water is remineralized by blending it with 5-10% brackish water. This means that desalinated water could easily have lithium concentrations of up to 100 ng/mL. Unlike contamination in some forms of drinking water, which might vary with factors like rainfall and industrial activity, we would expect lithium levels to be reliably high in desalinated water, because they are inherent to the source.
We even have some data about lithium levels in the waters of the Persian Gulf. Near Qeshm island, at least, seawater concentrations vary somewhat by season but are usually around 300 ng/mL. This is reasonably high for seawater and much higher than the levels usually observed in groundwater. Not all of that makes it back into the water after desalination, of course, but even if only 10% got back in, 30 ng/mL is still a pretty high dose to be receiving regularly.
(If you are a Kuwaiti or Saudi desalination engineer, please contact us! This blog has gotten 15 views from Kuwait and 26 from Saudi Arabia, we know you’re out there!)
In any case, if lithium from desalinated seawater doesn’t explain why the Middle East has such incredibly high rates of obesity, then some other explanation will have to be found for this extremely striking observation.
On average, people drink about 3 liters of water per day. If they’re drinking from a normal freshwater source with 1-10 ng/mL, they’ll get a dose of about 3-30 µg / day. If they’re drinking from desalinated seawater, with concentrations of about 30-100 ng/mL, they’ll get a dose of about 90-300 µg / day. If they’re drinking from sources like those found in Texas, Greece, and Mistelbach, with concentrations of about 100-200 ng/mL, they’ll get a dose of about 300-600 µg / day. If they’re drinking from sources like those found in Graz, Chile, and Argentina, with 1000 ng/mL, they’ll easily get a dose of 3000 µg / day or more:
In comparison, therapeutic doses are in the range of 1,000,000 µg per day, but remember the randomized controlled trial showed effects at only 400 µg per day. Many people are getting doses of similar amounts from their drinking water alone. And this is assuming that they’re not also exposed to lithium in other ways.
Common Uses of Lithium
Which they probably are, because lithium has a wide variety of applications. In 2017, the USGS estimated that 48% of the global market for lithium was batteries, 26% was ceramics and glass, 7% was lubricating greases, the remainder being industrial uses like polymer production and air treatment. They also mention a couple uses like “agrochemicals”, airbag ignition, aluminum alloys, cement and concrete additives, and dyes and pigments.
You’ll remember from our review in the PFAS section that some of the most obese professions include firefighters, cooks, food workers, cleaning workers, motor vehicle operators, vehicle mechanics, transportation and material moving, healthcare support, health technicians, and some construction occupations (“Helpers, construction trades” and “Other construction and related workers”).
If you go and see your local auto mechanic, the black smears covering his hands and forearms might be engine oil. But they might also be lithium grease. This grease is ubiquitous in auto engineering, routinely applied to hinges, joints, and pivot points. It’s used in aviation and on many kinds of heavy machinery, including logging and construction equipment, trains, and tractors. It also has a number of household applications. You might put it on your garage door, or the hinges on the gate of your fence. About 7% of the global supply of lithium goes into lubricating greases of one kind or another. That’s a lot of grease.
In addition to any lithium they’re exposed to in their food and water, vehicle mechanics, truck drivers, and transportation workers are also constantly exposed to lithium grease at work. They may literally be rubbing the grease all over their hands. Like any grease, this is hard to get off your skin, in most cases requiring a special soap. Hopefully they keep it out of their eyes and mouth, but even so, it doesn’t seem like it would be great for you.
Construction workers also use lithium grease to lubricate their tools and equipment. They may be exposed through lithium added to concrete and cement. Lithium is used in agrochemicals like pesticides, though information on exactly what agrochemicals this includes is spotty. It’s possible that this explains the higher levels of obesity in cooks and food workers.
Lithium grease isn’t considered food-safe, and in theory it shouldn’t be used on food-handling equipment. In practice, however, manufacturers and restaurants don’t always follow regulations. A quick Google search reveals incidents like lithium grease being stored with food equipment, lithium grease being stored next to garlic bulbs, and lithium grease being stored above mustard.
It’s not clear if there’s a connection with healthcare professionals, firefighters, or cleaning workers. Maybe there’s a hidden lithium connection out there. But there doesn’t have to be. Lithium may just be part of the story — the rest could be explained by other contaminants, like PFAS.
And speaking of PFAS, there’s actually a connection. Lithium greases often include other substances to improve their performance, including Teflon, aka PTFE.
Bioaccumulation
One strike against lithium as an explanation for the obesity epidemic is that it only stays in the body for a few days, with a half-life of 18-36 hours. The medical consensus seems to be that it probably doesn’t bioaccumulate.
But this may not be a problem, for a few reasons. First, lithium may be able to affect weight without accumulating in the body. One possible mechanism by which environmental contaminants could cause obesity is by interfering with the microbiome. If exposure to lithium changes the composition of your gut microbiota, then exposure to lithium could have serious impacts on your weight without any bioaccumulation. Even brief exposure to lithium could have long-lasting effects. And in fact there is evidence that dietary lithium affects the microbiome, at least in rats.
Second, the medical consensus might simply be wrong. While lithium is traditionally measured in the serum, this may not be the best way to evaluate bioaccumulation. “In contrast to other psychotherapeutic drugs,” says one paper on the pharmacokinetics of lithium, “Li+ is fairly evenly distributed in the body, but in tissues such as the white matter of the brain, the bones, and in the thyroid gland the concentrations per kg wet weight are about twice those in the serum.”
A particularly interesting example is a case study of a patient who died after lithium poisoning. Researchers found that most tissue samples (“liver, spleen, kidney, lung, muscle, cardiac muscle, pancreas”) contained about the same concentration of lithium as found in the serum, in the range of 0.4-0.6 mmol/kg. But in the thyroid gland and in brain tissue (especially white matter), lithium concentrations were nearly twice as high as in serum, in the range of 0.7-0.8 mmol/kg. They suggest that this is to be expected, saying, “lithium has an increased affinity to thyroid tissue,” and, “high concentrations of lithium in brain tissue – especially in white substance – agrees with investigations that reveal the lithium elimination from brain tissue to be slow.”
This is particularly interesting not only because it seems to show evidence of bioaccumulation, but because of the particular tissues in which concentrations were found to be highest. The thyroid gland is very important to weight regulation, and so to find that lithium concentrations in that organ were second-highest in the body is very neatly in line with our expectations. Maybe it shouldn’t be a surprise, because lithium therapy is associated with thyroid disease.
For a while this was the best evidence of lithium accumulation in the brain, but a few weeks ago our friend Dr. Grace Rosen sent us this Nature paper published in March 2021. In this paper, the authors took 139 brain samples from three deceased individuals and took them to a nuclear reactor in Bavaria, where they were placed in a chamber and shot with a “well focused beam of cold neutrons with a neutron flux of ɸ = 1.2 × 1010 cm−2 s−1”. The lithium-neutron interaction gives a unique “associated coincident energy pattern”, which allowed them to measure the amount of lithium at different sites in the brains. Unsurprisingly, the patient receiving lithium therapy at the time of death had the highest concentration, but the brains of the other two individuals did as well, presumably from trace exposure.
Just like the case study above, they found that lithium was more concentrated in white than in gray matter. Additionally, the authors note that lithium concentrations were especially high in the thalamus and Brodmann Area 25. This is interesting for our purposes because Brodmann Area 25 “influences changes in appetite and sleep” and the thalamus governs “sensory relay in visual, auditory, somatosensory, and gustatory systems.” Both of these brain regions are related to eating behavior.
Sadly the authors did not examine any samples from the hypothalamus, which governs eating more directly, but this is still evidence that trace lithium bioaccumulates in brain regions that are important to the regulation of food intake and body weight.
[Next Time: HIGHLIGHTS FROM THE COMMENTS]